This is an
excerpt from Dr. Norman Doidge in the January 22 2022 edition of the Globe and Mail. The full article is much longer - these are just the scientifically significant excerpts and references.
Norman Doidge, MD, is a psychiatrist, psychoanalyst and author of The Brain That Changes Itself. He is executive director of Health and the Greater Good.
In February, 2021, Pfizer’s CEO, Albert Bourla,
said the vaccine was still offering strong protection at the six-month mark and “indicators right now … are telling us that there is a protection against the transmission of the disease.” That April, Dr. Ugur Sahin, the CEO of BioNTech (which developed the vaccine for Pfizer),
told reporters, “Europe will reach herd immunity in July, latest by August.” It wasn’t a tough sell. Who would not want it to be true? Having no pandemic experience, we took them at their word. Politicians fostered the idea that our proper aim for handling COVID would be to “eliminate it everywhere,” as Prime Minister Justin Trudeau
said. Early treatment doesn’t promise that, though it might lower death rates. Eradication had more psychological appeal: let’s get it out of our lives forever.
Yet, in dismal December, 2021, two years in, with cases soon to reach record highs, and another lockdown looming and vaccines waning, it wasn’t working out that way. Perhaps if we hadn’t been so focused on one tool things might have gone differently. And perhaps if certain voices hadn’t been silenced, and others handed a megaphone, our pandemic tool kit, and mindset, would have been different too.
Early in the pandemic, at the Sainte-Anne site of the Parisian mental hospital, Psychiatrie & Neurosciences, something mysterious occurred. The staff started contracting COVID in high numbers, but their patients, gravely mentally ill, did not. Three staff got COVID for every patient, despite the patients having more risk factors, such as being overweight, or having cardiovascular disease.
Someone wondered, could it be that the patients’ psychiatric medications were protecting them? The staff homed in on chlorpromazine, a common antipsychotic medication, and learned it had antiviral properties against SARS-Cov-1 and MERS-CoV (the predecessors to SARS-CoV-2). In a May,
2020 publication, they proposed repurposing it for treating COVID-19.
French psychiatrists and scientists next did a
multicentre study, looking at 7,230 patients who had been hospitalized in Paris for severe COVID-19. Coincidentally, 300 of the patients were taking antidepressants. The data showed that those on Selective Serotonin Uptake Inhibitors (SSRI) – a kind of antidepressant – were less likely to require intubation or die. Not all SSRIs worked equally, but those that did reduced major inflammatory problems (the COVID “cytokine storm” that often kills).
Lab research showed that the SSRI fluvoxamine had an antiviral effect, and a salutary effect on blood platelets that might protect patients from blood clots.
Meanwhile, back in the U.S., in parallel process, a child psychiatrist, Dr. Angela Reirson, caught COVID in early 2020. Sick at home, she started doing research. She recalled a study on mice she had read the previous year. The mice had sepsis – a dangerous response to infection that can kill. Something akin to sepsis can happen in serious COVID. In the 2019 study, mice with sepsis were given fluvoxamine, which halted the condition. So, in March, 2020, Dr. Reirson contacted another psychiatrist, Eric Lenze, a colleague of hers at Washington University in St. Louis. Dr. Lenze was a specialist in repurposing drugs. Realizing fluvoxamine had a great safety record, he launched its first small randomized control trial of COVID patients. Not one of the 80 volunteers who got fluvoxamine deteriorated or got COVID lung damage, whereas 8 per cent of the 72 who got a placebo did deteriorate. The findings were published in
JAMA in November, 2020.
Next came the
Together Trial, the world’s largest placebo study of COVID drugs, co-led by McMaster researcher Edward Mills and Brazilian physician Gilmar Reis. To do large trials you need a lot of cases, and Brazil had two million. The study was published Oct. 27, 2021,
in the Lancet. It studied about 1,500 unvaccinated patients with COVID-19 who also had another serious illness and were at high risk for hospitalization. Half were given fluvoxamine, half a placebo. In those who took the fluvoxamine as prescribed it reduced the odds of hospitalization or emergency care by 66 per cent and death by 90 per cent.
The Ontario Science Table noticed these findings and on Dec. 20 it put fluvoxamine in the guidelines, for doctors to prescribe on an outpatient basis if needed, recognizing “the need for outpatient treatment options with a reasonable safety profile during an anticipated spike in COVID-19 cases due to the Omicron variant.”
That was significant, because early treatment of COVID – measures we can take to avoid symptomatic cases from worsening, requiring hospitalization – has been so minimal. In Ontario, treatment includes monoclonal antibodies (now only one
works with Omicron) for specific people at risk, and steroids. Otherwise outpatients were told to rest, drink fluids, and hope their immune system would handle the virus.
True, there was much talk of brand-new, non-repurposed drugs for early treatment. Pfizer’s Paxlovid, just approved by Health Canada on Monday, is very new. But repurposed drugs
have a track record, and thus often a safety advantage. And the generic ones are cheap. Fluvoxamine costs about $15 for a course of treatment. Repurposed drugs are used by poorer countries that can’t afford vaccines or expensive early treatment drugs such as Paxlovid ($500) or Molnupiravir (US$700 and not yet approved in Canada).
So why hasn’t treatment focused more on repurposed drugs?
First, because the master narrative, once it took hold, directed our attention away from this possibility. Second, in North America, the first repurposed drug that came to public attention was hydroxychloroquine. When it was endorsed by then-president Donald Trump it became highly politicized. People’s opinions about it often had more to do with their political affiliation than whether they had read any of the (now) 303 studies. Third,
agencies that regulate drugs, such as the U.S. Food and Drug Administration and Health Canada, mandate that any drug they evaluate have a sponsor, usually a drug company agreeing to assume liabilities for the drug. It’s an extremely expensive process. If an old, cheap generic drug shows promise for repurposing, it still needs a sponsor to get approved for that. But drug companies have no financial incentive to do so. So usually there are no sponsors, and the drugs languish.
There were “snake oil” claims on the internet, yes, but generally when scientists and health care workers were party to these quarrels, it was because there was a scientific debate. In such a case, to accuse one’s opponent of spreading “misinformation” is to pre-emptively ascribe to oneself an unjustified certainty – and to one’s opponent bad faith. At times no one really knew what was more harmful – e.g. keeping children out of school, or sending them in. There was incorrect information aplenty in our novel situation, and that included some spread by officials who flip-flopped multiple times on masks, or who, claiming to “follow the science,” differed with officials in similar jurisdictions, based on changing data.
The authors of the master narrative tend to say the main reason that things have not gone as they predicted is because variants arose. But if anything could have been predicted, it is that viruses mutate. Columbia virologist Vincent Racaniello described how fellow scientists were worried that the new mRNA technology, by focusing on only a small portion of the virus, the spike protein, would make it easy for the virus to “get around” or escape the vaccine through mutations. “That’s partly why,”
he said in May, “all the variants are arising now, because we have only the spike epitopes in there.” That view didn’t get much of a hearing.
It wasn’t just the variants’ role in declining vaccine efficacy that surprised people. There was something about the execution of the original clinical trials, conducted by the pharma companies themselves, on their own products that also led to this surprise. It’s worth going back for a moment and looking at how the problem unfolded.
In December, 2020, the new mRNA vaccines were rolled out, and were, according to the randomized clinical trials, 95 per cent (Pfizer) and 94.5 per cent (Moderna) efficacious in stopping infection. Physician-scientist Eric Topol, head of Scripps Labs,
said these vaccines “will go down in history as one of science and medical research’s greatest achievements.”
But by the time summer 2021 arrived, real world experience contradicted Mr. Bourla’s and Dr. Sahin’s claims of potency at six months, no transmission by the vaccinated, and imminent herd immunity. Pfizer’s Mr. Bourla, in his February interview, had called Israel “the world’s lab,” because it was vaccinated with the Pfizer extensively and several months ahead of other countries, giving the world a glimpse of its future. But when Israeli public health released its six-month data, they showed that vaccine effectiveness had dropped to 39 per cent, and Delta was surging. (The FDA had originally said it would
not approve a vaccine less than 50-per-cent effective.) A
Mayo clinic study showed that after six months, protection granted by the two Pfizer doses dropped from the original 95 per cent to 42 per cent. Another Israeli study showed it had dropped to
16 per cent. That huge discrepancy couldn’t be attributed just to the new variant, Delta, because protection was already
fading at five months for the earlier variants too.
So why such a discrepancy? The original studies were clinical trials. The
Pfizer study followed about 38,000 people without COVID who were divided in two groups – half got the vaccine, and half a placebo. The investigators asked the question: could the vaccines prevent symptomatic cases of COVID-19? But, as Peter Doshi, senior editor at the British Medical Journal,
warned, “None of the trials currently under way are designed to detect a reduction in any serious outcome such as hospital admissions, use of intensive care, or deaths.” He explained that, “Because most people with symptomatic COVID-19 experience only mild symptoms, even trials involving 30,000 or more patients would turn up relatively few cases of severe disease.” Susanne Hodgson of the University of Oxford agreed: “The current [randomized control trials] that are ongoing are … not powered to assess efficacy against hospital admission and death.
And how long had the Moderna and Pfizer vaccines been studied, when released for mass use in the winter of 2021? Two months.
These studies looked at the vaccines at their most potent, in a low risk population, and gave us a flattering snapshot. But COVID-19 is a movie.
In contrast, the Mayo study, and the Israeli data, were looking at data over a more realistic time course to test effectiveness.
The waning created a crisis in Israel. Dr. Sharon Alroy-Preis, director of Israel’s Public Health Services, told the FDA Vaccine Advisory Committee on boosters, why the country became the first to roll out a third shot: “What we saw prior to our booster campaign was that 60 per cent of people in severe and critical condition were immunized, doubly immunized, fully vaccinated and as I said, 45 per cent of the people who died in the fourth wave were doubly vaccinated.” Most “breakthrough infections” are indeed mild, but she was describing life-threatening ones in the vaccinated. As breakthrough infections became commonplace throughout the world, noted Harvard epidemiologist Michael Mina said, the message that “this is only an epidemic of the unvaccinated … is falling flat.”
As for Dr. Sahin’s claim that we were on the brink of vaccine-induced herd immunity and being rid of COVID altogether, experts such as Larry Brilliant (who had helped eradicate smallpox with vaccines) and five other scientists wrote in Foreign Affairs in July, 2021, “Among humans, global herd immunity, once promoted as a singular solution, is unreachable.” They explained in precise detail why COVID-19 was unlike smallpox, and it could not be “eradicated,” such as the fact it is growing in a dozen animal species already. “If we are forced to choose a vaccine that gives only one year of protection,” said Dr. Brilliant, “then we are doomed to have COVID become endemic, an infection that is always with us …” That vaccines would get us to a vaccine-based herd immunity had been one of the two main scientific justifications for vaccine mandates. Now it was gone.
The other justification for mandates had been that the vaccinated don’t transmit the virus.
Most of us had presumed, when we got our first doses, that we couldn’t pass the virus on to others. Public statements repeatedly praised people for “doing your part to stop the spread.” But in August, CDC director Rochelle Walensky told CNN, when asked why the vaccinated must wear masks, “Our vaccines are working exceptionally well. They continue to work well for Delta; with regard to severe illness and death, they prevent it. But what they can’t do any more is prevent transmission.”
In fact, the original randomized clinical trials for Pfizer and Moderna did not test if the vaccines stop transmission. Now our best hope was that the vaccinated might transmit less than the unvaccinated. Several studies could be interpreted as showing this. But others found the vaccinated likely had equal transmission. One study, conducted in a prison, concluded that the vaccinated prisoners had as much “transmission potential” as the unvaccinated prisoners, adding, “clinicians and public health practitioners should consider vaccinated persons who become infected with SARS-CoV-2 to be no less infectious than unvaccinated persons.” Dr. Cyrille Cohen, head of the immunotherapy lab at Bar-Ilan University, and adviser to the Israeli government on vaccine trials, said that with respect to transmission with Omicron, “we don’t see virtually any difference … between people vaccinated and nonvaccinated,” adding “both get infected with the virus, more or less at the same pace.” The rancour that we, the vaccinated, are increasingly directing against the unvaccinated, fuels itself by remaining wilfully oblivious of this later painful truth: we too spread, to ourselves, and to the unvaccinated, as they to us and each other.
These scientists maintain what matters is not whether a person is vaccinated or not, but whether they are immune or not. Thus, the European Union recognizes natural immunity in its Digital COVID Certificate, which is in lieu of a vaccine passport, and is not limited to proof of vaccination. You could get a passport and travel if you have been vaccinated or if you have “recovered from COVID-19″ or if you have a recent test saying you are negative. For air and train travel, Canada has also acknowledged recovery from COVID as an exemption, if one presents a recent negative test – but, inconsistently, natural immunity is not recognized in most other quasi-mandate situations here. Such scientists think it irrational that government calls for mass mandates are escalating just as the core original justifications for them – that the vaccinated don’t transmit the virus, and the vaccine will bring us to herd immunity – have collapsed.
Those unvaccinated people who were exposed to the virus, make up a huge number. For instance, in the U.S., according to a Columbia University study, by Jan. 31, 2021 (before many vaccines had been given) 10 months into the pandemic, 120 million Americans had natural immunity. Now, 12 months later, with the much more infectious Delta and Omicron variants, it is likely a highly significant majority of the unvaccinated now have natural immunity.
A recent pivotal study from South Africa – not yet peer reviewed – shows that in poor communities, where there was modest vaccination (39 per cent of adults), more than 70 per cent of people had already been exposed to the virus in previous waves, going into Omicron. The twice vaccinated had more protection than those who were unvaccinated and never had COVID. But the unvaccinated who had COVID and recovered had more protection from severe disease than the vaccinated. One Israeli study showed that the unvaccinated who recovered from COVID have 27 times less risk of reinfection compared with the vaccinated, and nine times less risk of hospitalization.
In a recent Munk Debate, Harvard’s Dr. Martin Kulldorff, an epidemiologist and vaccine safety specialist, argued that mandating vaccines for the naturally immune “actually creates problems because when people see that they are forced to take a vaccine that they don’t need because they already are immune, that causes a lot of distrust in public health. And we have seen during this last year and a half that all the hard work we’ve done over many decades to build trust in vaccines is now disappearing because we’re making these mandates that make no sense from a scientific or public health perspective.”
Israel’s third booster helped beat back the Delta wave. Then Omicron hit. On Dec. 19, The New York Times headlined an article, “Most of the World’s Vaccines Likely Won’t Prevent Infection from Omicron.” Thankfully, the vaccines still seemed like they would prevent those infections from becoming severe – the key point. A Kaiser study showed that two doses, over time, fell to zero efficacy against Omicron. Then Danish data showed that a booster offered protection against severe disease, but “only to those over 70 years.” But would boosters wane too? The U.K. Health Security Agency study showed the protection from the Pfizer booster (third shot) had dropped to 45-per-cent coverage at only 10 weeks.
We’ve had so many mood swings. We had been through a year of defining vaccine success as eliminating the virus, then as lowering infection and stopping the spread, to discovering there were breakthrough infections and transmission to other people, but that they still lowered our risk of hospitalization and death – that’s worth a lot – though not always in the most vulnerable. In the West, many have responded to waning vaccine protection with time by doubling down, proposing ever more boosters. What is the scientific evidence for frequent boosters? That’s a matter of scientific debate.
The original Pfizer study submitted to the FDA booster meeting was shockingly tiny – a mere 306 patients were given the section, and they had been followed for only a month, and, again, most of the subjects were younger than those at risk (18-55). Pfizer wanted it on that basis rolled out to millions. That was enough to get FDA officials asking hard questions. Crucially, nobody had studied the long-term effects of multiple mRNA boosters – there hasn’t been time. The FDA refused Pfizer’s recommendation to approve the booster for the entire U.S. population, with the top two heads of its Vaccine Research and Review Committee, Dr. Marion Gruber, (the head, and former acting chief scientist at the FDA), and Philip Krause (deputy director), and international colleagues, writing in the Lancet:
“There could be risks if boosters are widely introduced too soon, or too frequently, especially with vaccines that can have immune-mediated side-effects (such as myocarditis, which is more common after the second dose of some mRNA vaccines, or Guillain-Barre syndrome, which has been associated with adenovirus-vectored COVID-19 vaccines [like the AstraZeneca or Johnson & Johnson]). If unnecessary boosting causes significant adverse reactions, there could be implications for vaccine acceptance that go beyond COVID-19 vaccines.”
When the head scientists of the FDA Vaccine Review committee and colleagues raise such questions, it can’t be dismissed as fringe fear-mongering. Shortly after, Dr. Gruber and Dr. Krause quit the FDA because the Biden administration was putting pressure on them to approve boosters before the vaccine committee had even met. The standard practice for approval is for the agencies to convene panels of outside experts to review the data openly, weigh risks and benefits, and take votes. But in December, the FDA and CDC leadership three times took the extraordinary step of not convening those experts for key booster meetings, in essence going around them because committee members had warned that the science supporting boosters for younger people was weak to non-existent, and they had safety concerns. Dr. Paul Offit, perhaps the most high profile provaccine physician-scientist in America, who was on the FDA panel told The Atlantic, he wouldn’t advise a booster for his healthy son in his 20s, or a healthy male in his teens, because the risks of myocarditis (higher in males) outweigh the benefits. Dr. Offit rejects the CDC’s and FDA’s all-or-nothing approach to children’s vaccination.
Vinayak Prasad, the UCSF epidemiologist, says if you put the Danish, Ontario, U.S., and Kaiser studies about Omicron together, “it’s time to face the reality about the vaccines.”
“Two doses of vaccine does nothing or almost nothing to stop symptomatic SARS-CoV-2,” he says. “Three doses barely does anything, and the effect will likely attenuate over time.” He says, “Booster mandates make no sense. … Boosting should happen in populations where it further reduces severe disease and death – a.k.a. older and vulnerable people.”
With Omicron surging, Israeli public health met to discuss a fourth booster. The New York Times reported that some scientists on the Israeli government booster advisory panel, “warned that the plan could backfire, because too many shots might cause a sort of immune system fatigue, compromising the body’s ability to fight the coronavirus.” This immune system fatigue was, perhaps, not inconsistent with negative vaccine efficacy. It’s not proven, but the fact that public-health officials were voicing such concerns shows that the doubling down strategy on boosters is being reappraised on safety lines. The EU, in a reversal, has just come out against regular, continuing boosters, saying they are afraid it will weaken the immune system.
Just as deaths have decoupled from cases with Omicron, our COVID mandates have decoupled from the science originally used to justify them. But the goalposts are moving, and now it is argued that only mandates will keep hospitals free of high-risk unvaccinated patients. What are the numbers? As of Jan. 20, there are 740 unvaccinated, and 2,091 fully vaccinated people in hospital for COVID (but not the ICU). In the ICUs there are 208 unvaccinated and 263 fully vaccinated people. True, there are fewer unvaccinated than vaccinated people in Ontario, but if surgeries are delayed, it is clearly because both groups are occupying beds. Portraying the unvaccinated as the sole cause is inaccurate, and deflects from the painful fact that Canada has fewer ICU and acute care beds per capita than almost any country in the developed world, and that the current vaccines are not working as well as hoped. What is called for is not more scapegoating and coercion, but healing, and more early treatment for both groups, now that we have it. Honouring the bedrock of medical ethics, no treatment without consent, is humane, preferable and possible.
Also reappraising is Bill Gates himself. He admitted this past November, “We need a new way of doing the vaccines.” He also accepted that our focus had been too narrow. “We didn’t get much in the way of therapeutics … way less than should have been the case.”
Consider how different our narrative is now. More and more officials are saying openly what the authors of the Great Barrington Declaration – the ridiculed view of 60,000 public health scientists and physician signatories – said some time ago: Our goal is not eradication of the virus, or a one-size-fits-all policy, but lessening of deaths in the vulnerable through focused protection, and focused vaccination. The immunity we have will be a mix of vaccine immunity and natural immunity, depending on the person. The new plan – to live with the virus and get back to living a normal life – is a departure from the pure Baconian “conquest of nature,” and hearkens back to the ancient, Hippocratic, notion that we must work with nature as an ally, in a kind of collaboration.
Since nature can indeed be both “the enemy,” but also is our very foundation, and potential ally and friend, no narrative that excludes either side of this friend and foe duality can ever do justice to medicine and healing. If the abandonment of Hippocrates was the first medical reversal, we are seeing in its return, a reversal of a reversal.
It’s been a blow to our Baconian narcissism to be upended by nature these past two years. That thin-skinned Baconian within seems almost offended to admit that protection has come not only from scientific advances, but from natural immunity. Others might see this as a reassuring reminder that natural processes are not always and only the enemy. We shall find out, as we observe the unvaccinated, to what extent natural immunity, accumulating in waves of infection over time, does or does not protect, for the current or future variants.
Till then, let’s give infallibility the day off. We have some ingenuity and some tools in our tool kit, none perfect, but if we use the whole kit, instead of just the hammer, we might be better for it. That goes for how we treat the virus, and how we treat each other. And for those scientists among us – those strange creatures, always reappraising! – there is comfort in knowing that after two years of hard work, we have a new narrative, or picture of our situation, which though imperfect, is more nuanced and likely closer to the truth.
|
Pfizer’s CEO, Albert Bourla, said the vaccine was still offering strong protection at the six-month mark and “indicators right now … are telling us that there is a protection against the transmission of the disease.
Bourla said current data shows that after six months the protection is robust.
"But there are a lot of indicators right now that are telling us that there is a protection against the transmission of the disease," Bourla added.
|
Ugur Sahin of BioNTech (which developed the vaccine for Pfizer) said the EU could see herd immunity by July or August 2021
Europe can achieve herd immunity against the coronavirus this summer, the head of the German pharmaceutical company BioNTech, said on Wednesday.
"Europe will reach herd immunity in July, latest by August,'' Ugur Sahin, BioNTech's chief executive, told reporters.
While the precise threshold required to reach that level of immunization is still under debate, experts say a level above 70% would significantly disrupt transmission of the virus within a population.
|
"To eliminate COVID-19 anywhere, we need to eliminate it everywhere" - JT
Justin Trudeau
@JustinTrudeau
Officiel du gouvernement - Canada
To eliminate COVID-19 anywhere, we need to eliminate it everywhere. I’ve said those words before and, during today’s working session at the @G7, we focused on how we can do that - and on how, together, we can make sure no one gets left behind as we recover.
|
Inhibition of the replication of SARS-CoV-2 in human cells by the FDA-approved drug chlorpromazine
Urgent action is needed to fight the ongoing COVID-19 pandemic by reducing the number of infected people along with the infection contagiousness and severity. Chlorpromazine (CPZ), the prototype of typical antipsychotics from the phenothiazine group, is known to inhibit clathrin-mediated endocytosis and acts as an antiviral, in particular against SARS-CoV-1 and MERS-CoV. In this study, we describe the in vitro testing of CPZ against a SARS-CoV-2 isolate in monkey and human cells. We evidenced an antiviral activity against SARS-CoV-2 with an IC50 of ∼10μM. Because of its high biodistribution in lung, saliva and brain, such IC50 measured in vitro may translate to CPZ dosage used in clinical routine. This extrapolation is in line with our observations of a higher prevalence of symptomatic and severe forms of COVID-19 infections among health care professionals compared to patients in psychiatric wards. These preclinical findings support the repurposing of CPZ, a largely used drug with mild side effects, in COVID-19 treatment.
|
Association between antidepressant use and reduced risk of intubation or death in hospitalized patients with COVID-19
We examined the potential usefulness of antidepressant use in patients hospitalized for COVID-19 in an observational multicenter retrospective cohort study conducted at AP-HP Greater Paris University hospitals.
|
The serotonin reuptake inhibitor Fluoxetine inhibits SARS-CoV-2
To circumvent time-consuming clinical trials, testing whether existing drugs are effective inhibitors of SARS-CoV-2, has led to the discovery of Remdesivir. We decided to follow this path and screened approved medications “off-label” against SARS-CoV-2. In these screenings, Fluoxetine inhibited SARS-CoV-2 at a concentration of 0.8µg/ml significantly, and the EC50 was determined with 387ng/ml. Fluoxetine is a racemate consisting of both stereoisomers, while the S-form is the dominant serotonin reuptake inhibitor. We found that both isomers show similar activity on the virus. Fluoxetine treatment resulted in a decrease in viral protein expression. Furthermore, Fluoxetine inhibited neither Rabies virus, human respiratory syncytial virus replication nor the Human Herpesvirus 8 or Herpes simplex virus type 1 gene expression, indicating that it acts virus-specific. We see the role of Fluoxetine in the early treatment of SARS-CoV-2 infected patients of risk groups.
|
Fluvoxamine vs Placebo and Clinical Deterioration in Outpatients With Symptomatic COVID-19
In this randomized trial that included 152 adult outpatients with confirmed COVID-19 and symptom onset within 7 days, clinical deterioration occurred in 0 patients treated with fluvoxamine vs 6 (8.3%) patients treated with placebo over 15 days, a difference that was statistically significant.
|
Preventing death and improving health outcomes for all people affected by COVID-19.
The TOGETHER Trial represents an international collaboration of diverse partners committed to preventing death and improving health outcomes for all people affected by COVID-19. Watch this brief video to better understand the important and innovative work that we are engaged in.
|
Effect of early treatment with fluvoxamine on risk of emergency care and hospitalisation among patients with COVID-19: the TOGETHER randomised, platform clinical trial
Treatment with fluvoxamine (100 mg twice daily for 10 days) among high-risk outpatients with early diagnosed COVID-19 reduced the need for hospitalisation defined as retention in a COVID-19 emergency setting or transfer to a tertiary hospital.
|
All but one monoclonal antibody treatments fail against omicron.
Treatments Fail Against Omicron
The single remaining monoclonal antibody therapy effective against the variant is now in short supply in the U.S., imperiling an option that doctors and hospitals have relied on.
|
Dozens of re-purposed drugs for COVID
List of a number of therapeutic agents and how the evidence stacks up for or agaist their use in treating COVID-19.
|
that's partly why all the variants are arising now, because mRNA shots only have the spike epitopes in there
must say that early in the outbreak last year, when the vaccine development was just ramping up, we talked a lot about this idea that, should they really only be focusing on spike? Shouldn't they be putting some other viral proteins on, and in retrospect it was a good decision to get vaccines out in less than a year, because otherwise it might've been more complicated. But that's partly why all the variants are arising now, because we have only the spike epitopes in there. And so it's easy for the virus to get around that. So, it's two ways, that story. So those are the things that we've talked about.
And also, I should say, we talked a long time about antivirals and whether they would play a role. And, we looked at remdesivir and how it was given so late in infection. And we said, this is not gonna work, it's too late. That's an inflammatory disease, later in infection. And it turned out remdesivir, yes, it doesn't work if you give it in the inflammatory phase. And now we actually don't have any useful antivirals, and the monoclonals can be effective, but again, you can't give them when someone's in an ICU, you have to hit them before. And we've just learned that. And these are some of the things we've talked about over the months.
Makary: Interesting. You know, I'm really interested in what you said about whether or not the spike protein was the right thing to target in the vaccines -- and it turns out it was very effective. Because I was having this conversation with one of my colleagues who does a lot of immunology research. And I asked the question -- I like to put big questions out there to have a discussion -- and the question was, do you think natural immunity or vaccinated immunity is stronger, and which one's more durable, two different domains. And I'd love your thoughts on that. But one interesting thing he said was he thought that maybe natural immunity, if you really get sick and you've got to mount a big antibody response, may be better because your body is developing antibodies and memory to all of the surface of the virus, not just the spike protein, and that may be better immune protection.
Racaniello: I think it's an interesting question and there's no one answer because every virus is slightly different. For example, the human papillomavirus, the vaccines we have make amazing immunity, better than immunity you get from natural infection, because there's so much protein in those vaccines. And you end up having great mucosal immunity, which is what you need there. On the other hand, other vaccines allow infection without disease. Of course, the polio vaccines were only tested to prevent polio, not to prevent infection. That's all we cared about.
Now for SARS-CoV-2, yes, having other proteins in the mix is a good idea. I think it depends on the severity of the disease. We did a paper 6 months ago which studied people who had died from COVID. So this was a very serious disease. And their lymph nodes had no germinal centers, which means no memory B cells to SARS-CoV-2. Even though they had antibodies, they had very low affinity antibodies.
And so the outcome of that was the idea that if you have a very serious disease, then you're not likely to have a long memory response. Now, those are people who died. So we don't know how it applies to people who have lived because they were able to take out their lymph nodes and study them. And it's not so easy to do in people who have survived. So a natural infection can have consequences. So, on the one hand, yes, you make a lot of viral proteins and those are great epitopes for mainly T cells because I think most of the antibodies that are going to block infection are going to be spike directed. But any other viral protein could in theory be a T-cell target. So you'll get more epitopes.
The counter view is that the virus may encode immune antagonists that could alter the immune response in some way that's not as good as, say, a vaccine. So it really depends. And we don't know enough yet. So I think if people are making a blanket statement that natural infection is always better, that's not always correct. It really depends on the virus.
|
Physician-scientist Eric Topol, head of Scripps Labs, said these vaccines “will go down in history as one of science and medical research’s greatest achievements.”
This will go down in history as one of science and medical research's greatest achievements. Perhaps the most impressive.
|
The FDA had originally said it would not approve a vaccine less than 50-per-cent effective.
The FDA's cutoff for Covid-19 vaccine effectiveness is 50 percent. What does that mean?
No vaccine is 100 percent effective, but some work better than others.
|
A Mayo clinic study showed that after six months, protection granted by the two Pfizer doses dropped from the original 95 per cent to 42 per cent.
Although clinical trials and real-world studies have affirmed the effectiveness and safety of the FDA-authorized COVID-19 vaccines...
|
Another Israeli study showed vaccine protection had dropped to 16 per cent.
Israeli lawmakers are keen to avoid another lockdown after overseeing one of the world's fastest vaccination drives. New daily coronavirus infections, however, have just climbed to record levels.
|
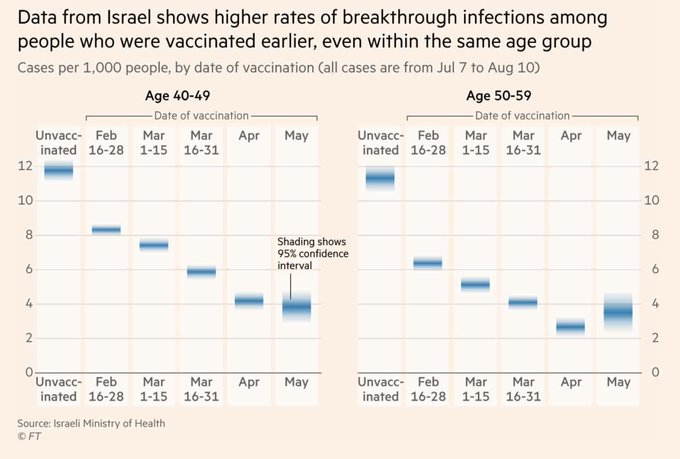
protection was already fading at five months for the earlier variants
And a graph of higher rates of breakthrough over time in Israel
|
The Pfizer study followed about 38,000 people without COVID
Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine
|
Will covid-19 vaccines save lives? Current trials aren’t designed to tell us - most people with symptomatic COVID-19 experience only mild symptoms
As phase III trials of covid-19 vaccines reach their target enrolments, officials have been trying to project calm. The US coronavirus czar Anthony Fauci and the Food and Drug Administration leadership have offered public assurances that established procedures will be followed.1234 Only a “safe and effective” vaccine will be approved, they say, and nine vaccine manufacturers issued a rare joint statement pledging not to prematurely seek regulatory review.5
But what will it mean exactly when a vaccine is declared “effective”? To the public this seems fairly obvious. “The primary goal of a covid-19 vaccine is to keep people from getting very sick and dying,” a National Public Radio broadcast said bluntly.6
Peter Hotez, dean of the National School of Tropical Medicine at Baylor College of Medicine in Houston, said, “Ideally, you want an antiviral vaccine to do two things . . . first, reduce the likelihood you will get severely ill and go to the hospital, and two, prevent infection and therefore interrupt disease transmission.”7
Yet the current phase III trials are not actually set up to prove either (table 1). None of the trials currently under way are designed to detect a reduction in any serious outcome such as hospital admissions, use of intensive care, or deaths. Nor are the vaccines being studied to determine whether they can interrupt transmission of the virus
|
Moderna vaccine only studied for two months before release
Vaccines and Related Biological Products Advisory Committee Meeting
December 17, 2020
FDA Briefing Document
Moderna COVID-19 Vaccine
|
Pfizer vaccine only studied for two months before release
Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine
|
Israel’s head of public health services, said the summer’s rise in the number of hospitalized patients who had been fully vaccinated with Pfizer’s vaccine was “scary.”
Dr. Sharon Alroy-Preis, Israel’s head of public health services, said the summer’s rise in the number of hospitalized patients who had been fully vaccinated with Pfizer’s vaccine was “scary.” She said 60 percent of severely or critically ill patients and 45 percent of those who died during what she called the fourth surge had received two injections of Pfizer’s vaccine.
After offering boosters to the general population, she said, Israel was now averaging about half as many severe or critically ill patients as anticipated.
|
"45 per cent of the people who died in the fourth wave were doubly vaccinated"
ADVISORY COMMITTEE MEETING
Vaccines and Related Biological Products Advisory Committee September 17, 2021 Meeting Announcement
SEPTEMBER 17, 2021
|
|
|
|
"global herd immunity, once promoted as a singular solution, is unreachable. Rather than die out, the virus will likely ping-pong back and forth across the globe for years to come.”
It is time to say it out loud: the virus behind the COVID-19 pandemic is not going away. SARS-CoV-2 cannot be eradicated, since it is already growing in more than a dozen different animal species. Among humans, global herd immunity, once promoted as a singular solution, is unreachable. Most countries simply don’t have enough vaccines to go around, and even in the lucky few with an ample supply, too many people are refusing to get the shot. As a result, the world will not reach the point where enough people are immune to stop the virus’s spread before the emergence of dangerous variants—ones that are more transmissible, vaccine resistant, and even able to evade current diagnostic tests. Such supervariants could bring the world back to square one. It might be 2020 all over again.
Rather than die out, the virus will likely ping-pong back and forth across the globe for years to come. Some of yesterday’s success stories are now vulnerable to serious outbreaks. Many of these are places that kept the pandemic at bay through tight border controls and excellent testing, tracing, and isolation but have been unable to acquire good vaccines. Witness Taiwan and Vietnam, which experienced impressively few deaths until May 2021, when, owing to a lack of vaccination, they faced a reversal of fortune. But even countries that have vaccinated large proportions of their populations will be vulnerable to outbreaks caused by certain variants. That is what appears to have happened in several hot spots in Chile, Mongolia, the Seychelles, and the United Kingdom. The virus is here to stay. The question is, What do we need to do to ensure that we are, too?
|
CDC director Rochelle Walensky told CNN vaccines do not prevent transmission.
“Our vaccines are working exceptionally well. They continue to work well for Delta; with regard to severe illness and death, they prevent it. But what they can’t do any more is prevent transmission.” (Note: they never ever did prevent infection and transmission - RJS)
|
coronaviruses do not tend to trigger long-lasting immunity
A chief concern is that coronaviruses do not tend to trigger long-lasting immunity. About a quarter of common colds are caused by human coronaviruses, but the immune response fades so rapidly that people can become reinfected the next year.
Researchers at Oxford University recently analysed blood from recovered Covid-19 patients and found that levels of IgG antibodies – those responsible for longer-lasting immunity – rose steeply in the first month of infection but then began to fall again.
Last week, scientists at Rockefeller University in New York found that most people who recovered from Covid-19 without going into hospital did not make many killer antibodies against the virus.
“That’s what is particularly challenging,” says Stanley Perlman, a veteran coronavirus researcher at the University of Iowa. “If the natural infection doesn’t give you that much immunity except when it’s a severe infection, what will a vaccine do? It could be better, but we don’t know.” If a vaccine only protects for a year, the virus will be with us for some time.
Another challenge: making any vaccine safe
In the rush to develop a vaccine – there are now more than 100 in development – safety must remain a priority. Unlike experimental drugs for the severely ill, the vaccine will be given to potentially billions of generally healthy people.
This means scientists will have to check extremely carefully for signs of dangerous side-effects. During the search for a Sars vaccine in 2004, scientists found that one candidate caused hepatitis in ferrets. Another serious concern is “antibody-induced enhancement” where the antibodies produced by a vaccine actually make future infections worse. The effect caused serious lung damage in animals given experimental vaccines for both Sars and Mers.
Hopes for eliminating the virus start with a vaccine but do not end there. “If and when we have a vaccine, what you get is not rainbows and unicorns,” says Larry Brilliant, CEO of Pandefense Advisory, who worked on the WHO’s smallpox eradication programme. “If we are forced to choose a vaccine that gives only one year of protection, then we are doomed to have Covid become endemic, an infection that is always with us.”
The virus will still be tough to conquer with a vaccine that lasts for years.
“It will be harder to get rid of Covid than smallpox,” says Brilliant. With smallpox it was at least clear who was infected, whereas people with coronavirus can spread it without knowing. A thornier problem is that as long as the infection rages in one country, all other nations are at risk.
|
the original randomized clinical trials for Pfizer and Moderna did not test if the vaccines stop transmission
The New York Times ran several articles on this, reporting that AstraZeneca, Pfizer, and Moderna had each withheld their study protocols from outside scientists and the public. Withholding protocols guarantees that outside researchers can’t know how participants are selected or monitored, and how effectiveness or safety are defined, so they can’t really know what exactly is being studied.
|
“clinicians and public health practitioners should consider vaccinated persons who become infected with SARS-CoV-2 to be no less infectious than unvaccinated persons.”
A total of 978 specimens were provided by 95 participants, of whom 78 (82%) were fully vaccinated and 17 (18%) were not fully vaccinated. No significant differences were detected in duration of RT-PCR positivity among fully vaccinated participants (median: 13 days) versus those not fully vaccinated (median: 13 days; p=0.50), or in duration of culture positivity (medians: 5 days and 5 days; p=0.29). Among fully vaccinated participants, overall duration of culture positivity was shorter among Moderna vaccine recipients versus Pfizer (p=0.048) or Janssen (p=0.003) vaccine recipients.
As this field continues to develop, clinicians and public health practitioners should consider vaccinated persons who become infected with SARS-CoV-2 to be no less infectious than unvaccinated persons. These findings are critically important, especially in congregate settings where viral transmission can lead to large outbreaks.
|
"lower probability of infectious virus detection in respiratory samples of vaccinated HCWs with breakthrough infections compared to unvaccinated HCWs with primary SARS-CoV-2 infections."
Background SARS-CoV-2 vaccines are highly effective at preventing COVID-19-related morbidity and mortality. As no vaccine is 100% effective, breakthrough infections are expected to occur.
Methods We analyzed the virological characteristics of 161 vaccine breakthrough infections in a population of 24,706 vaccinated healthcare workers (HCWs), using RT-PCR and virus culture.
Results The delta variant (B.1.617.2) was identified in the majority of cases. Despite similar Ct-values, we demonstrate lower probability of infectious virus detection in respiratory samples of vaccinated HCWs with breakthrough infections compared to unvaccinated HCWs with primary SARS-CoV-2 infections. Nevertheless, infectious virus was found in 68.6% of breakthrough infections and Ct-values decreased throughout the first 3 days of illness.
Conclusions We conclude that rare vaccine breakthrough infections occur, but infectious virus shedding is reduced in these cases.
|
“we don’t see virtually any difference … between people vaccinated and nonvaccinated,” adding “both get infected with the virus, more or less at the same pace.”
Israeli vaccine advisor: “We have made mistakes”
Professor Cyrille Cohen talks herd immunity and his pandemic regrets
Cohen is head of Immunology at Bar Ilan University and a member of the advisory committee for vaccines for the Israeli Government. In a wide-ranging and forthright interview, the Professor tells Freddie Sayers:
The Green Pass / vaccine passport concept is no longer relevant in the Omicron era and should be phased out.
He and his colleagues were surprised and disappointed that the vaccines did not prevent transmission, as they had originally hoped.
The biggest mistake of the pandemic in Israel was closing schools and education
Omicron has accelerated the pandemic into the endemic phase, in which Covid will be “like flu”
Especially with Omicron, where we don’t see virtually any difference, there is a very narrow gap between people vaccinated and non-vaccinated, both can get infected with a virus, more or less at the same pace.
- CYRILLE COHEN, UNHERDTV
|
it is likely a highly significant majority of the unvaccinated now have natural immunity
INFECTIOUS DISEASE Feb. 09 2021
Active COVID Cases May Be Ten Times Official Count: Study
The number of active COVID-19 cases in the United States is roughly ten times higher than the number of confirmed cases on any given day, according to a computer model by Columbia University Mailman School of Public Health scientists. Since the start of the pandemic, an estimated one-third of the U.S. population has already been infected, with numbers five times that of the official count.
Jeffrey Shaman, PhD, a professor of environmental health sciences known for his COVID-19 projections, led the research, based on case numbers and anonymized cellphone location data to estimate population mixing. The findings appear ahead of peer review in a report by NPR.
At the worst day of the pandemic so far, on January 2, 91 out of every 100,000 people in the U.S. tested positive. In fact, 998 per 100,000 people were actively shedding the virus on that day, according to the study’s estimates. In some areas, this discrepancy was even more profound: In Los Angeles, at the peak of the winter surge, 3 percent of the county’s population was infectious, or roughly 3,000 per 100,000.
|
mandating vaccines for the naturally immune “actually creates problems because when people see that they are forced to take a vaccine that they don’t need because they already are immune, that causes a lot of distrust in public health
“If we want to have long-term trust in public health, we cannot use coercion and mandates. We have to use education and mutual trust.”
|
Israel’s third booster helped beat back the Delta wave.
TEL AVIV, Israel - Israel, which last summer was the first country to offer wide-scale coronavirus booster shots, announced this week that it will roll out a fourth-dose campaign, again offering other nations a potential glimpse into their pandemic future as the omicron variant spreads across the globe.
|
Most of the World’s Vaccines Likely Won’t Prevent Infection From Omicron
A growing body of preliminary research suggests the Covid vaccines used in most of the world offer almost no defense against becoming infected by the highly contagious Omicron variant.
All vaccines still seem to provide a significant degree of protection against serious illness from Omicron, which is the most crucial goal. But only the Pfizer and Moderna shots, when reinforced by a booster, appear to have initial success at stopping infections, and these vaccines are unavailable in most of the world.
The other shots — including those from AstraZeneca, Johnson & Johnson and vaccines manufactured in China and Russia — do little to nothing to stop the spread of Omicron, early research shows. And because most countries have built their inoculation programs around these vaccines, the gap could have a profound impact on the course of the pandemic.
|
two doses, over time, fell to zero efficacy against Omicron
6657 test positive cases (44% delta, 56% omicron) were included. The 2-dose VE against omicron infection was 30.4% (95% CI, 5.0%-49.0%) at 14-90 days after vaccination and declined quickly thereafter. The 3-dose VE was 95.2% (93.4%-96.4%) against delta infection and 62.5% (56.2%-67.9%) against omicron infection. The 3-dose VE against omicron infection was low among immunocompromised individuals (11.5%; 0.0%-66.5%). None of the cases (delta or omicron) vaccinated with 3 doses were hospitalized compared to 53 delta and 2 omicron unvaccinated cases.
|
Danish data showed that a booster offered protection against severe disease, but “only to those over 70 years.”
Though 2 & 3 doses of vax not effectively preventing infection, 2 doses evidently protecting against severe disease & death in adults & 3 doses seem to offer extra protection in those >70
|
The U.K. Health Security Agency study showed the protection from the Pfizer booster (third shot) had dropped to 45-per-cent coverage at only 10 weeks.
SARS-CoV-2 variants of concern and
variants under investigation in
England
Technical briefing 33
23 December 2021
(PDF)
|
“There could be risks if boosters are widely introduced too soon, or too frequently, especially with vaccines that can have immune-mediated side-effects (such as myocarditis, which is more common after the second dose of some mRNA vaccines, or Guillain-Barre syndrome, which has been associated with adenovirus-vectored COVID-19 vaccines [like the AstraZeneca or Johnson & Johnson]). If unnecessary boosting causes significant adverse reactions, there could be implications for vaccine acceptance that go beyond COVID-19 vaccines.
If unnecessary boosting causes significant adverse reactions, there could be implications for vaccine acceptance that go beyond COVID-19 vaccines. Thus, widespread boosting should be undertaken only if there is clear evidence that it is appropriate.
|
Dr. Gruber and Dr. Krause quit the FDA because the Biden administration was putting pressure on them to approve boosters before the vaccine committee had even met
Two Top F.D.A. Vaccine Regulators Are Set to Depart During a Crucial Period
The announcement that Dr. Marion Gruber and Dr. Philip Krause will leave this fall comes as the agency conducts sensitive reviews of coronavirus vaccines for children and booster shots.
|
In December, the FDA and CDC leadership three times took the extraordinary step of not convening those experts for key booster meetings, in essence going around them because committee members had warned that the science supporting boosters for younger people was weak to non-existent, and they had safety concerns.
The Biden administration has been sidelining vaccine experts
The FDA, for example, approved booster shots for 16- and 17-year-olds without convening a key advisory panel
|
Dr. Paul Offit, perhaps the most high profile provaccine physician-scientist in America, who was on the FDA panel told The Atlantic, he wouldn’t advise a booster for his healthy son in his 20s, or a healthy male in his teens, because the risks of myocarditis (higher in males) outweigh the benefits. Dr. Offit rejects the CDC’s and FDA’s all-or-nothing approach to children’s vaccination.
Should Teen Boys Get Boosted?
Third shots for adolescent boys and young men were already a hard sell. Then came Omicron.
|
“Two doses of vaccine does nothing or almost nothing to stop symptomatic SARS-CoV-2,”
It Is Time to Face Reality about the Vaccines
A number of studies are converging on the fact that 2 doses of vaccination has poor vaccine effectiveness against Omicron. 3 doses does slightly better, but the effect will rapidly wane as antibody titers fall, and infection is certain as the number of exposures increase. These studies have immediate implications for vaccine and health-care policies.
First, Kaiser Southern California. Here are data for 2 doses of mRNA for effectiveness against Omicron. Follow the red line. Over time, it is 0%.
|
As of Jan. 20, there are 740 unvaccinated, and 2,091 fully vaccinated people
Graphs and tables of COVID-19covid 19 hospitalization data by status, location and number of people in the ICU.
|
Our goal is not eradication of the virus, or a one-size-fits-all policy, but lessening of deaths in the vulnerable through focused protection, and focused vaccination. The immunity we have will be a mix of vaccine immunity and natural immunity, depending on the person.
The view of 60,000 public health scientists and physician signatories
|
We shall find out, as we observe the unvaccinated, to what extent natural immunity, accumulating in waves of infection over time, does or does not protect, for the current or future variants.
61% of the world population has received at least one dose of a COVID-19 vaccine.
10.08 billion doses have been administered globally, and 22.67 million are now administered each day.
Only 10% of people in low-income countries have received at least one dose.
Our international COVID-19 vaccination dataset is updated each morning (London time), with data up to the previous day.
|
|
|